Cholera
Cholera is an acute intestinal infection caused by the aquatic bacterial species Vibrio cholerae. Transmission is due to oral or fecal-oral contact and outbreaks are mainly linked to poor hygiene and a lack of clean water. Most people will have relatively mild infections, yet vulnerable people like pregnant women or young children have a higher chance of severe illness. Once patients are infected the toxin produced by the cholera bacteria can cause large quantities of watery diarrhea with high electrolyte concentrations. Due to the large loss of fluids, patients can develop hypovolemia and ultimately shock which can lead to death. Therefore, it is important to ensure patients receive treatment focusing on re-hydration using oral rehydration solution in milder cases or large amounts of intravenous fluids in more severe cases.
Source: Lancet https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(03)15328-7/fulltext
Climate sensitive infectious diseases
Increased greenhouse gas emissions cause global warming which leads to changes in precipitation patterns, sea level rise, storms, floods, droughts, heatwaves and changes in natural cover. Climate sensitive infectious diseases are aggravated by these changes in the earth’s climate. More than half (58%) of infectious diseases confronted by humanity worldwide have been or will be aggravated by climatic hazards. Emergence of a disease depends on pathogens and people coming into contact, and the extent to which peoples’ resistance is diminished, or the pathogen is strengthened, by a climatic hazard. An overview of how climate change impacts infectious disease in different manners is shown in the figure.
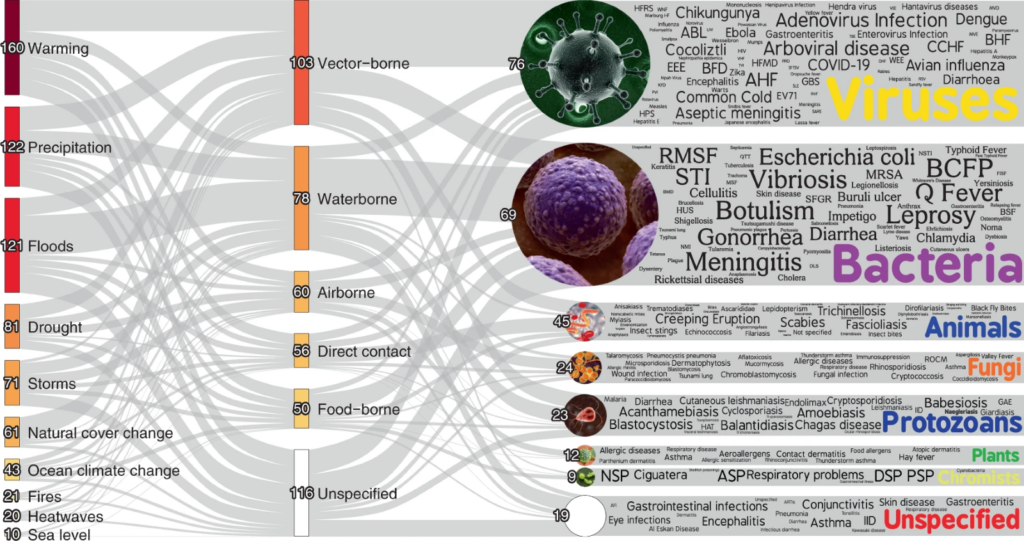
Source: Mora et al, 2022 Nature Climate Change https://www.nature.com/articles/s41558-022-01426-1
Cholera as example of climate sensitive infectious disease
While some of the triggers for cholera outbreaks—like poverty and conflict—are enduring, climate change is now increasing the problem. Climate change leading to ocean warming, ocean acidification, rising sea levels and changes in salinity due to precipitation changes all have been found to increase the risk of cholera for multiple regions in the world. Extreme climate events like floods, cyclones and droughts reduce access to clean water and sanitation, which creates an ideal environment for cholera to thrive. Therefore, Cholera is an example of an infectious disease that is aggravated by climate change.
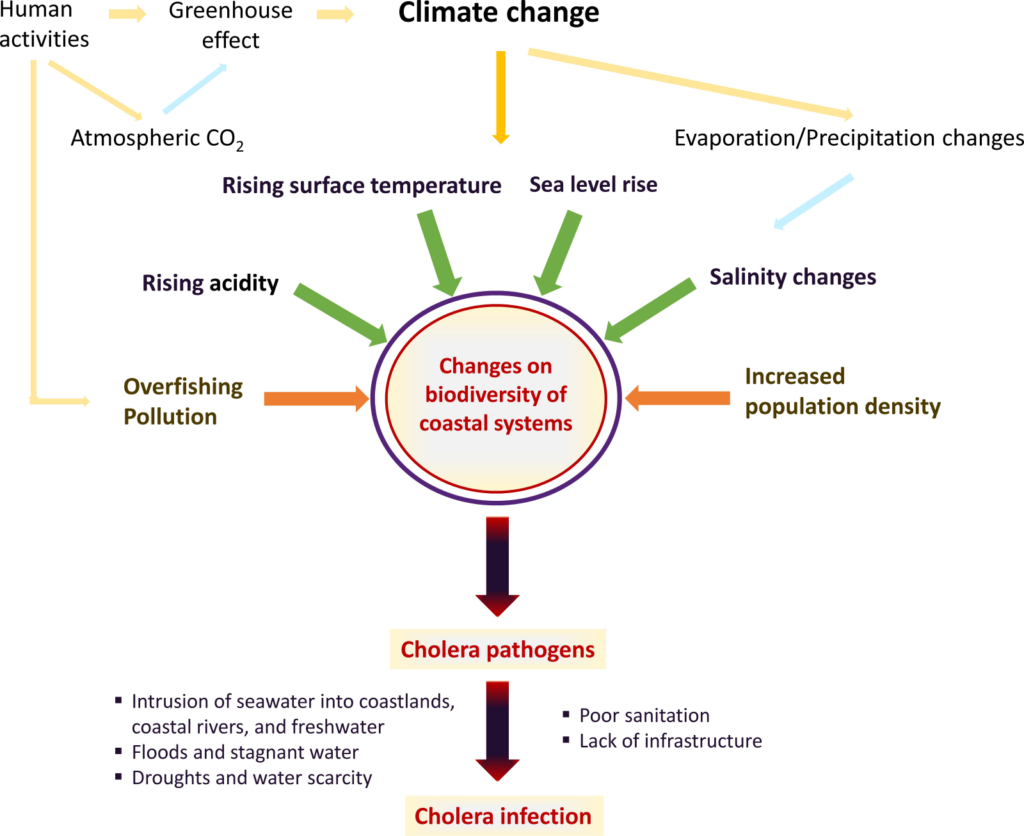
Sources: Christaki E, Dimitriou P, Pantavou K, Nikolopoulos GK. The Impact of Climate Change on Cholera: A Review on the Global Status and Future Challenges. Atmosphere. 2020; 11(5):449. https://doi.org/10.3390/atmos11050449 , Cholera upsurge (who.int)
Antibiotics
Antibiotics usually help shorten the duration of illness in an individual patient and therefore reduces the needed amount of fluids. It may limit the time of cholera excretion, but in an epidemic setting like this there will be a limited impact on the amount of people infected. This is mainly due to many cases likely being mild and not seeking care, but still excreting bacteria. There is a risk of resistance forming if mass-prophylaxis is provided.
Vaccine
Different oral cholera vaccines are available. It takes time for effective immunity to build up after a second dose, therefore a cholera vaccine will have very limited direct effects on containing an outbreak.
Vector-borne disease and climate change
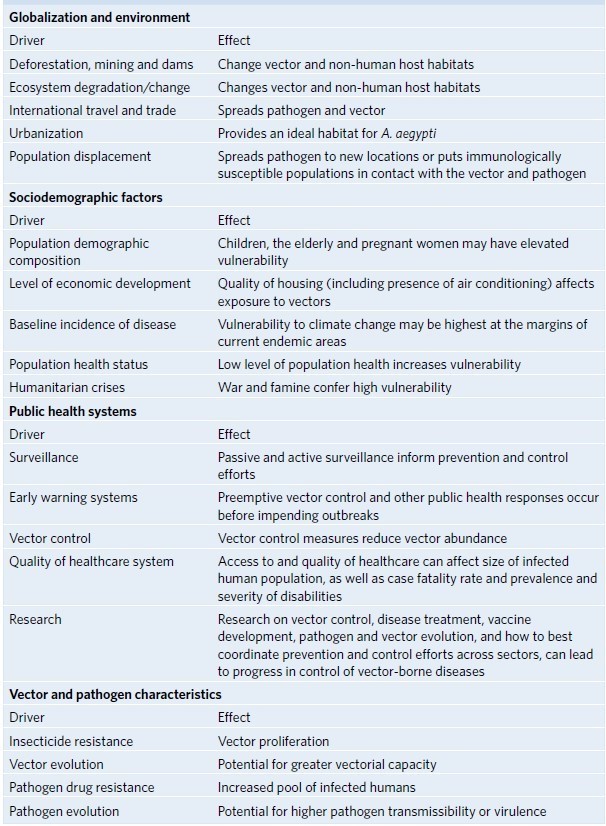
Dengue is a vector-borne disease: Tiger mosquitos of the Aedes species (the vectors) transmit a virus (Dengue) to humans that causes the dengue fever infection. Geographical distribution of dengue depends on the mosquito habitat. Climate change, affecting precipitation patterns, average temperatures and humidity, may increase the risk of an outbreak by affecting this habitat. This holds true not only for dengue, but for the entire class of vector-borne diseases, such as malaria, Zika or Tick-borne Encephalitis. Due to climate change, suitable habitats for mosquitos have expanded and the population of Aedes mosquitos has increased worldwide by 10% since the 1950’s. This is, however, not directly linked to infectious disease patterns, and each disease may be affected in a different way. Other, non-climate factors have an effect on the transmission and spread of vector-borne diseases:
Table from: Rocklöv, J., Dubrow, R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat Immunol 21, 479–483 (2020). https://doi.org/10.1038/s41590-020-0648-y
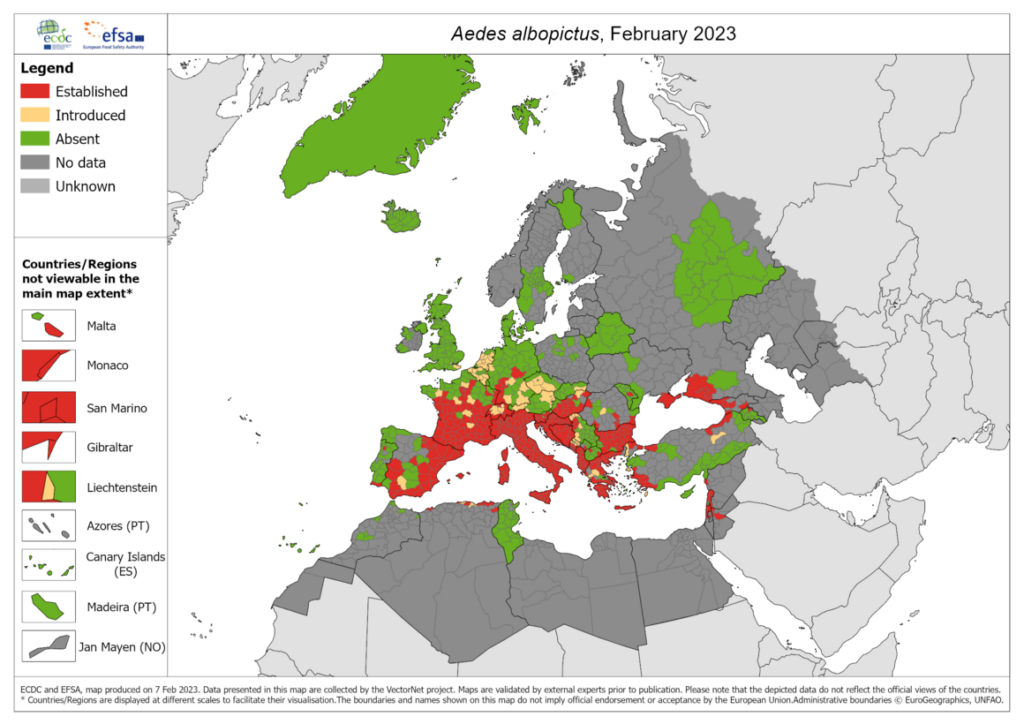
Tiger mosquito
In this figure from the European Centre for Disease Prevention and Control you can study the current distribution of Aedes mosquitos in Europe, which have a potential to cause dengue fever outbreaks. As you can see the mosquito is established in most southern European countries and is getting introduced in more northern European countries.
Climate change adaptation
To adapt to the changing climate and weather patterns we will have to know the predicted effects of climate change on our weather. For northern Europe this will in general lead to more heatwaves during summer and more intense rain causing a higher risk of flooding. Examples of adapting to climate change are building floodwater dams to adapt to these more extreme weather events. If planned well, adaptation measure can have co-benefits, such as green roofs green roofs to reduce the urban heat island effect can also increase biodiversity and mental health.
Nature based solutions
“Nature-based Solutions (NbS) are actions to protect, sustainably manage and restore natural and modified ecosystems in ways that address societal challenges effectively and adaptively, to provide both human well-being and biodiversity benefits.” (IUCN, 2016) NbS examples are reforestation, wetland restoration and green infrastructure. These solutions can be used as alternatives to ‘grey/conventional’ infrastructure to address a societal challenge like adapting to more extreme weather due to climate change by using nature to get both infrastructure (co-)benefits as supporting biodiversity and improve air and water quality. Yet, NbS can also lead to dis-benefits by providing a habitat for vectors that could transmit disease.
From a Planetary Health perspective where human-, animal- and ecosystem health are all connect, an elegant solution for many current health issues may be to tap into nature’s own solutions using biomimicry and nature-based solutions.

What is AMR?
Antimicrobial resistance (AMR) is the ability of microorganisms, such as bacteria, to become increasingly resistant to an antimicrobial to which they were previously susceptible. AMR is a consequence of natural selection and genetic mutation. Such mutation is then passed on conferring resistance. This natural selection process is exacerbated by human factors such as inappropriate use of antimicrobials in human and veterinary medicine, poor hygiene conditions and practices in healthcare settings or in the food chain facilitating the transmission of resistant microorganisms. Over time, this makes antimicrobials less effective and ultimately useless.
One health concept
One Health is an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems. It recognizes that the health of humans, domestic and wild animals, plants, and the wider environment (including ecosystems) are closely linked and interdependent. One health touches upon many of the same issues as in Planetary Health, but generally focusses more on infectious diseases and the links between human and animal health. By linking humans, animals and the environment, One Health can help to address the full spectrum of disease control – from prevention to detection, preparedness, response and management – and contribute to global health security.
Source: https://www.who.int/health-topics/one-health#tab=tab_1
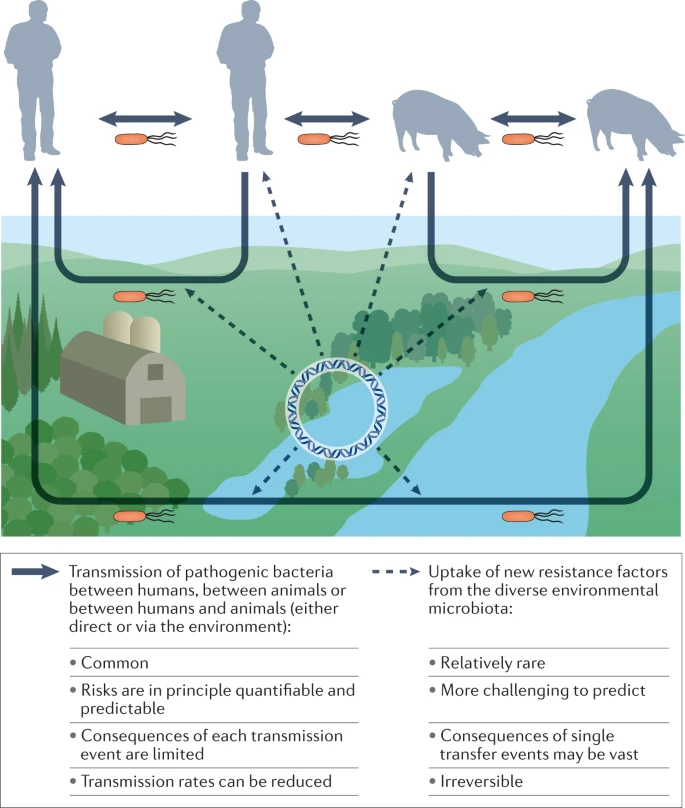
AMR in the environment
The main routes for transmission of resistant pathogens are between humans, between domestic animals and sometimes between animals and humans. These transmission routes can be direct or indirect via the external environment (lower part of the figure), often through faecal contamination. These events are with already resistant pathogens. However, new resitant bacteria can also form by horizontal gene transfer from the diverse, environmental microbiota (dashed arrows). Such transfer events may occur either in the environment or within the human or domestic animal microbiota. The consequences of single gene transfer events may be vast and are irreversible, leading to the emergence of a new resistant bacterium.
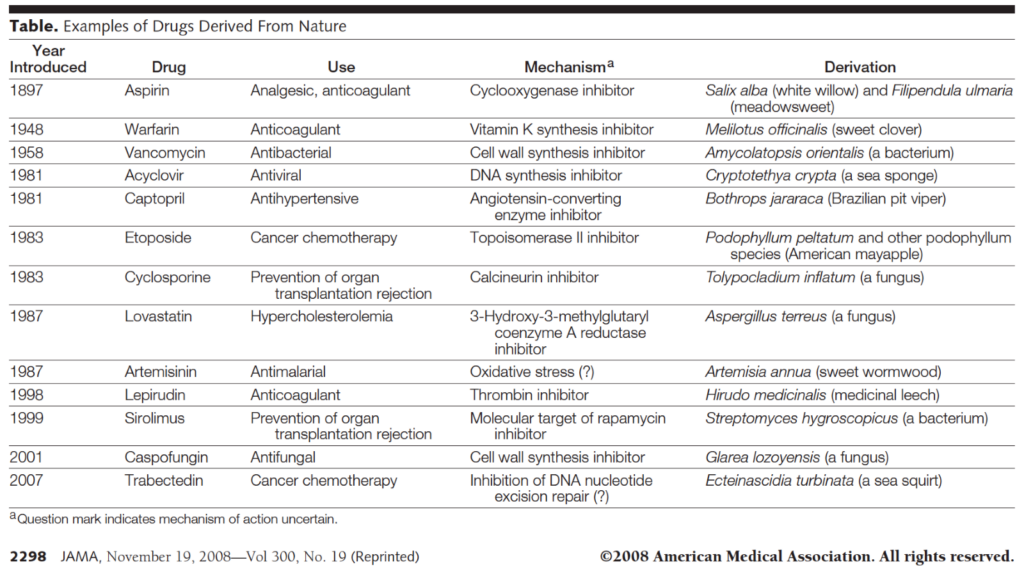
Biodiversity as a source of (antimicrobial) drugs
Loss of biodiversity has a direct effect on medicine: 50-80% of all pharmaceuticals are derived from nature or based on a naturally occurring molecule. This is particularly true for antibiotics, which are often produced by natural enemies of certain bacterial species, such as fungi or competing bacterial strains. In the face of rising antimicrobial resistance, it is crucial to identify novel antibiotics, for which likely many options are still available in ecosystems around the world that have not yet been discovered. However, with an extinction rate estimated to be 100-1000x higher than it would have been in the absence of humans, we will probably lose many potential pharmaceuticals before they can even be discovered.
Sloths, living in tropical rainforests under threat by deforestation, are an interesting example of the variety of potential pharmaceuticals to be discovered. Fur isolates from a single population of sloths revealed 84 types of fungi, many of which targeted the parasites causing malaria and Chagas disease, as well as 20 potential antibiotics, of which one had an entirely novel mechanism of action.
Further reading:
Connecting global priorities: Biodiversity & Human Health report, Chapter 9
Bernstein, The importance of biodiversity to medicine. JAMA 2008; https://jamanetwork.com/journals/jama/article-abstract/182891
Sloth paper: Higginbotham et al. PLoS One 2014; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3893167/
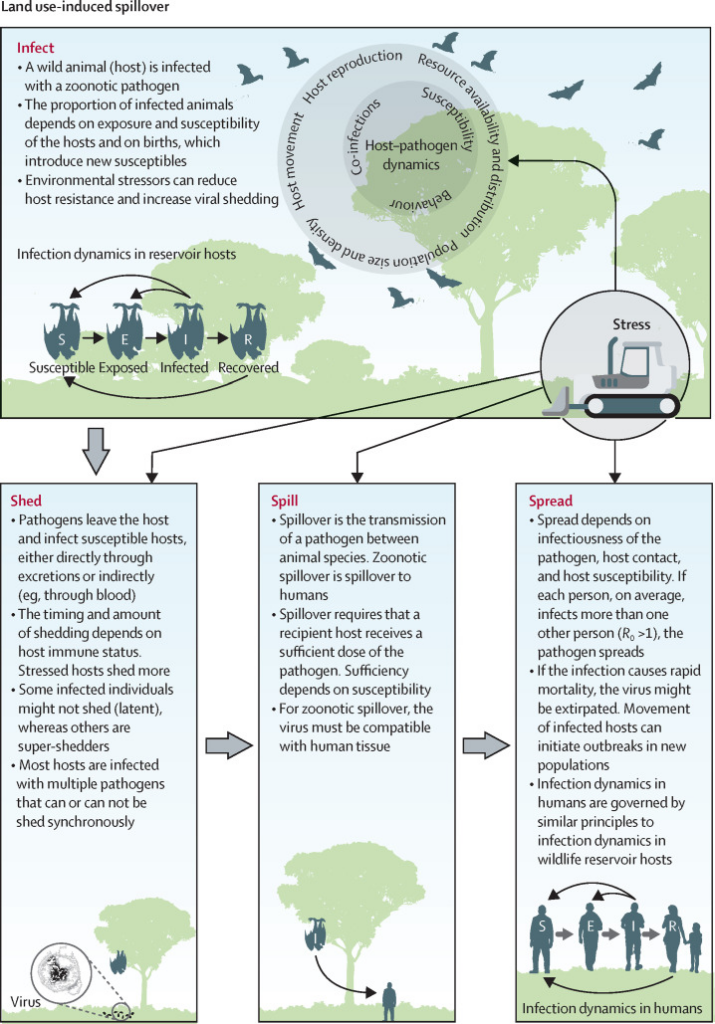
What is a spillover event?
Zoonotic spillover occurs when a pathogen, like a virus or bacteria, transfers from animals to humans, potentially leading to new infectious diseases outbreaks. These events can occur through direct contact with animals, consumption of contaminated animal products, or via vectors like mosquitoes or ticks. Examples include COVID-19 (from bats), HIV/AIDS (from primates), and Avian Influenza (from birds).
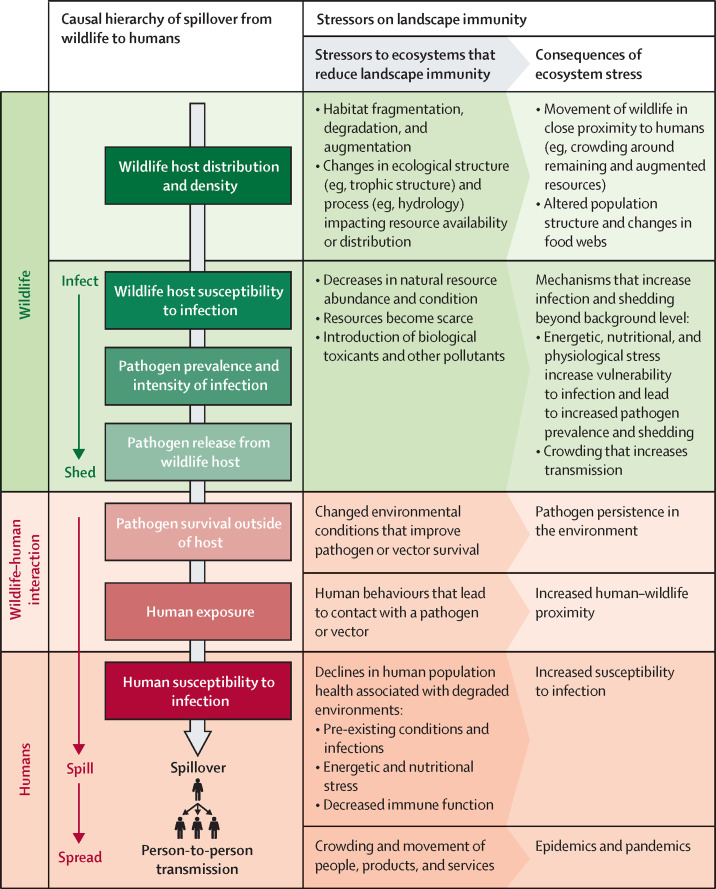
Drivers of disease emergence/spillover
Emerging infectious disease outbreaks are driven by a complex interplay of environmental, biological, and societal factors. Rapid urbanization, population growth, and land-use changes, such as agricultural expansion, increase human-wildlife interactions, creating opportunities for zoonotic spillovers.
One of the primary drivers is land-use change, which alters ecosystems and brings wildlife, humans, and livestock into closer contact. This increased interaction heightens the risk of zoonotic spillover, where pathogens jump from animals to humans. Deforestation, agricultural expansion, and urbanization are key examples of land-use changes that disrupt natural habitats, stressing wildlife populations and increasing their susceptibility to infections whilst bringing humans closer into contact with potential vectors.
Climate change also plays a significant role by altering the distribution of disease vectors like mosquitoes and ticks, thereby expanding the range of infectious diseases. Furthermore, global travel and trade can rapidly spread pathogens across regions, turning local outbreaks into global pandemics. An incremental increase in air travel and human mobility contributes to the swift international transmission of diseases like SARS-CoV-2. These dynamics are further exacerbated in densely populated urban areas, where poor living conditions and increased human connectivity accelerate the spread of infectious diseases
Human behavior, such as wildlife trade and consumption, also contributes to the risk of disease emergence. Markets selling live animals provide ideal conditions for pathogens to cross species barriers.
To mitigate these risks, a holistic approach that considers ecosystem health, wildlife conservation, and human health is essential.
Sources:
